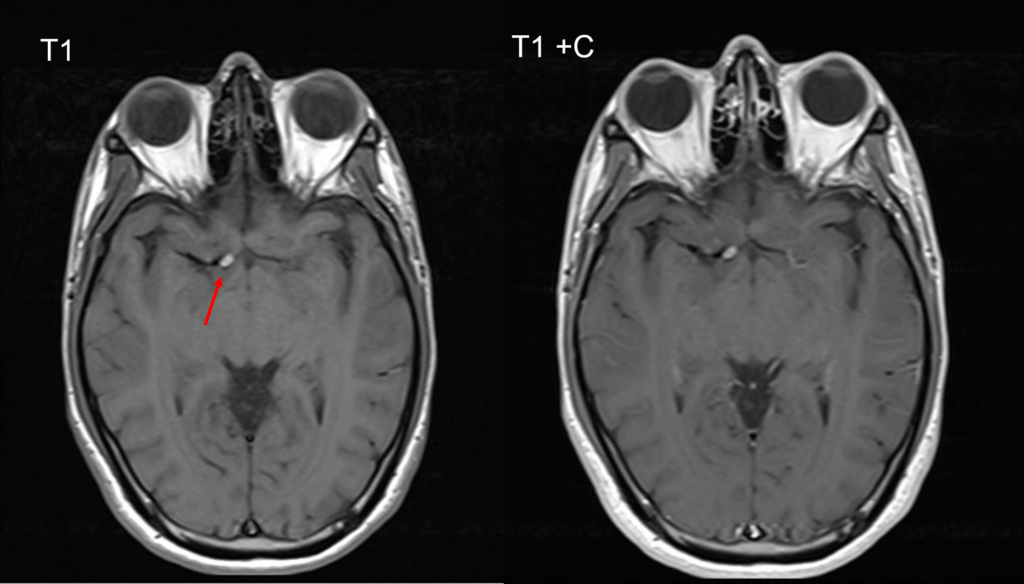
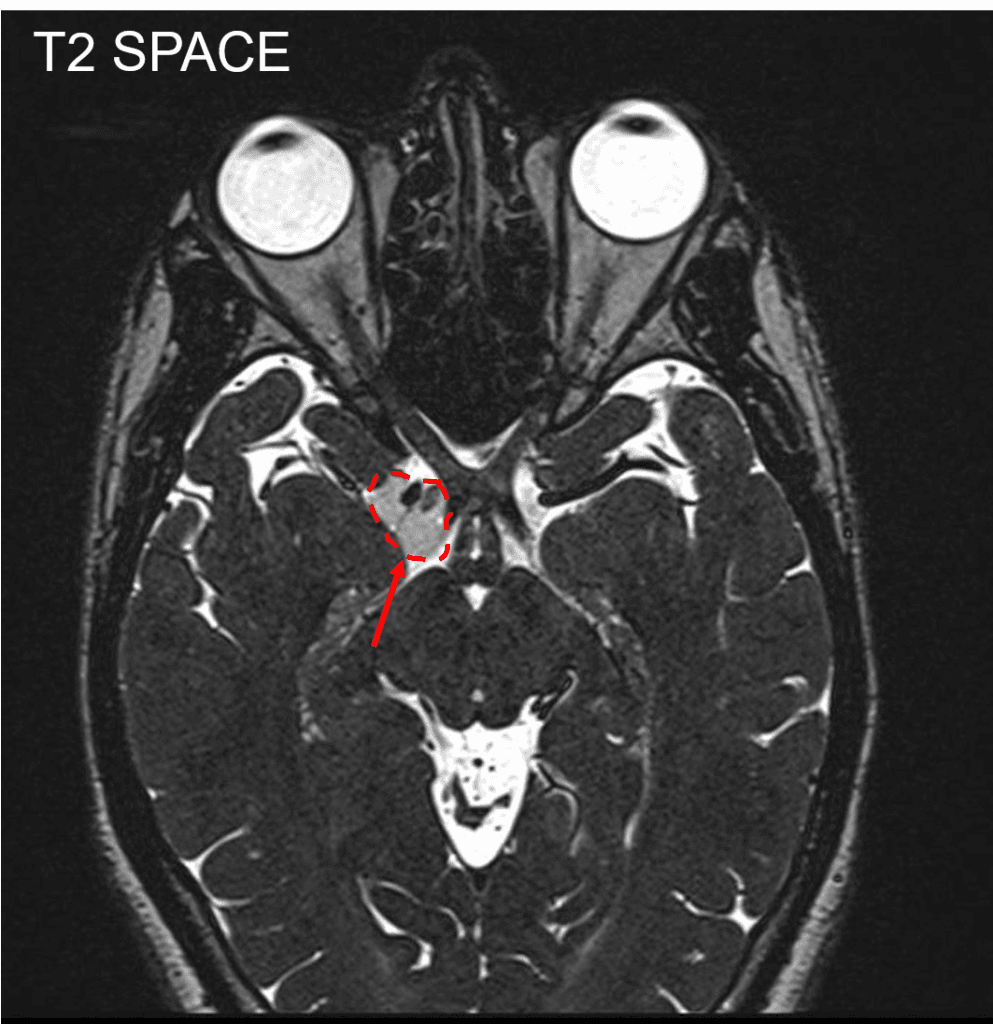
Patient with a 1 year history of worsening diplopia, headaches, and dizziness. MRI demonstrates a suprasellar mass in the right supraclinoid cistern with compression CN III. A right pterional craniotomy was performed to approach the supraclinoid/suprasellar region. A cyst was encountered and subsequently fenestrated. Pathology was consistent with a dermoid.
History & Physical
Young male with a 1 year history of worsening diplopia, headaches, and dizziness. MRI demonstrates a suprasellar mass in the right supraclinoid cistern with compression CN III. No neurologic deficit on exam.
Radiographic Findings
Surgery
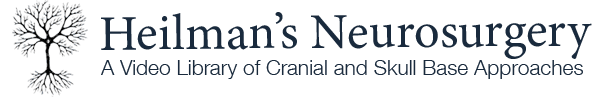
A skin incision was made starting in front of the right tragus and extending up behind the hairline to the midline in the frontal region. The incision was carried down to the plane above the temporalis fascia. The periosteum was cleaned off the frontal bone. A subfascial incision was made, and the scalp was reflected anteriorly over gauze rolls using spring-loaded fishhooks. A cuff of temporalis fascia and muscle was left attached to the skull at the origin of the temporalis muscle for reattachment at the end of the case. The temporalis muscle was dissected up out of the temporalis fossa and retracted laterally.
The Midas Rex drill was used to make several bur holes along the outline of the planned pterional craniotomy bone flap, and these holes were then connected with the footplate attachment. A standard right pterional bone flap was elevated off the dura and set aside in antibiotic solution. We did not enter the frontal sinus. The sphenoid wing and the inner table of the frontal bone were drilled down flush with the anterior cranial fossa. Excellent hemostasis was obtained.
The dura was opened in a curvilinear fashion and tacked up anteriorly using 4-0 Nurolon sutures. The operative microscope was brought into use. The arachnoid over the sylvian fissure was opened with microscissors, and the sylvian fissure was split from a lateral to medial direction. As CSF was released, the brain became nicely relaxed.
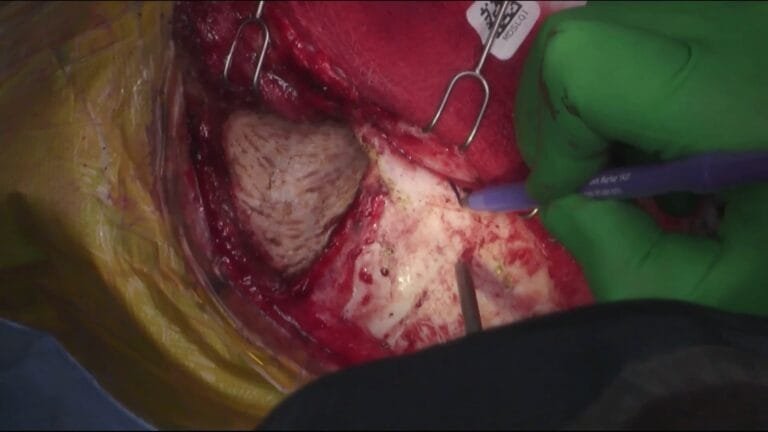
As we approached the carotid cistern, we could see a cyst containing green, mucus-like material in the carotid cistern. The Budde Halo retractor system was used to gently support the frontal lobe away from the anterior cranial fossa. The arachnoid over the right optic nerve was opened, and the frontal lobe was dissected off the right optic nerve. The arachnoid over the carotid cistern was opened, and the posterior communicating artery, anterior choroidal artery, and the tentorial edge were identified.
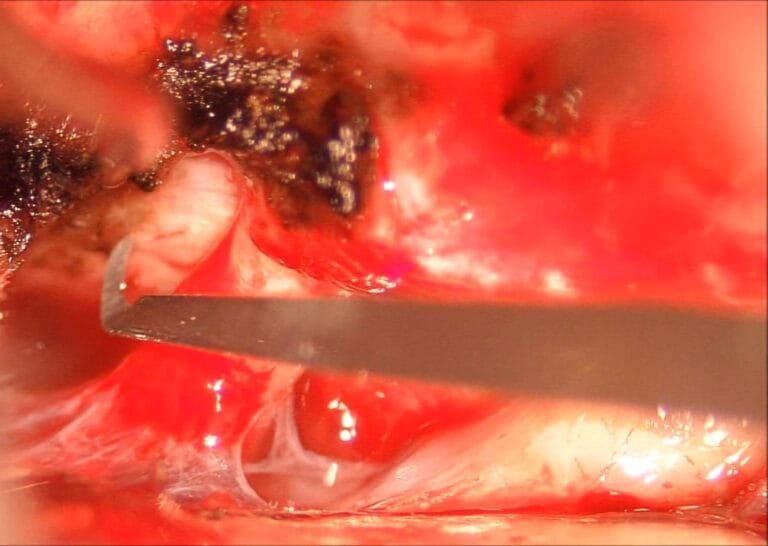
A cystic structure was seen surrounding the posterior aspect of the supraclinoid carotid. A small opening was made into the cyst, and it was full of green, mucus-like material, similar to that found in colloid cysts. The cyst contents were suctioned out. The entire cyst was then dissected out using microsurgical techniques. It was dissected off the undersurface and posterior aspect of the supraclinoid carotid and gradually dissected off the anterior choroidal artery. Arachnoid adhesions were divided with microscissors.
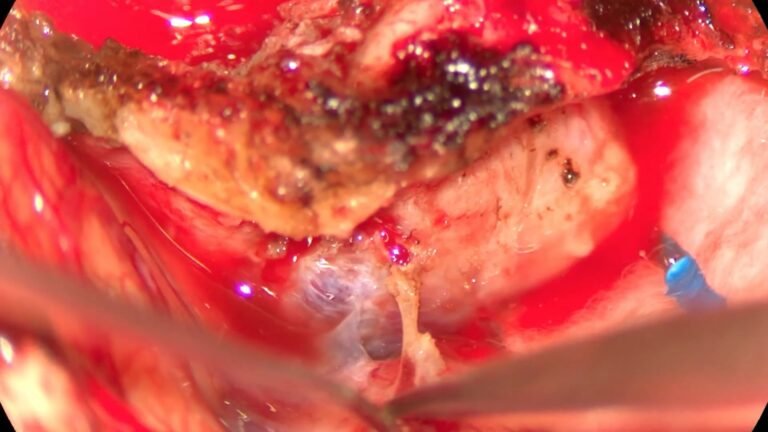
The cyst was knuckling into the third cranial nerve just as it entered the ocular motor cistern. Using microscissors, the cyst was sharply cut off the third cranial nerve from an anterior to posterior direction until the entire cyst was removed in one piece. The entire cyst was removed. The basal cisterns were irrigated with warm Ringer’s lactate solution. The Budde Halo retractor system was removed, and the dura was closed using interrupted and running 4-0 Nurolon sutures. Surgicel was placed over the dura, and the bone flap was secured back into place using Stryker Leibinger titanium miniplates.
The crevices around the bone flap were filled with hydroxyapatite bone cement. The temporalis muscle was sutured back to its origin, and the temporalis fascia was sutured back to the temporalis muscle. The scalp was closed after irrigation with antibiotic solution using 3-0 Vicryl for the galea and staples for the skin edges.